Leg arteriogram
A leg arteriogram is an imaging test that uses x-rays and a special dye to see inside the arteries in the leg. The purpose is to diagnose and see any blockages or stenoses (narrowing). This may be performed on one, or both legs.
Once an arteriogram has been completed, and a blockage or stenosis has been confirmed, if it is appropriate, treatment can commence. Treatment options include angioplasty, stenting, lithoplasty or atherectomy. Your interventional radiologist will determine which treatment is best suited for you.
Angioplasty
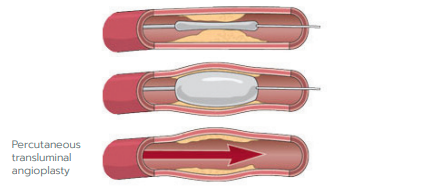
Percutaneous Transluminal Angioplasty (PTA) is the opening of a stenosed (narrowed) or blocked blood vessel using a balloon catheter. The balloon inflates to a specific size, forcing the blood vessel to expand.
In most cases the artery will remain open following the balloon inflation, and, in most instances, a drug coated balloon will then be utilised to help stop the narrowing returning. Sometimes however, the artery does not respond well to a balloon catheter, and in that case, the next step would be to place a stent in the artery.
Stenting
If an angioplasty has been unsuccessful, or a recurrent stenosis persists, a stent will then be inserted so the artery can remain patent.
A stent used in the artery is a metal, mesh like tube made from either nitinol (nickel-titanium alloy) or cobalt chromium. Alternatively, it can be covered with a material, such as polytetrafluoroethylene (ePTFE). Your interventional radiologist or vascular surgeon will decide on the type of stent depending on your specific circumstance, and the location of the blockage.
