Left atrial appendage (LAA) closure 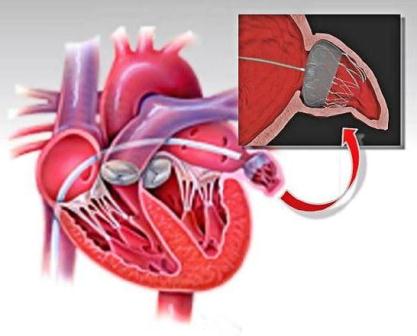
This is a treatment to prevent stroke caused by blood clots forming in the left atrial appendage in patients who suffer from atrial fibrillation (AF) and other factors that increase the risk of stroke, particularly if they have difficulty managing blood thinning therapy.
Patients who have artificial heart valves or who are likely to need valve replacement may not be suitable.
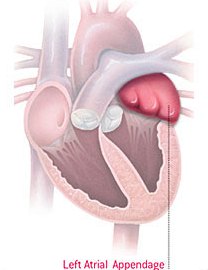
The left atrial appendage is a small, windsock-like pouch, which empties into the left atrium of the heart.
For patients with normal heart rhythm, the left atrial appendage squeezes rhythmically with the rest of the left atrium. This rhythmic contraction ensures that blood in the pouch is ejected when the left atrium empties into the left ventricle, where it is then pumped all over the body.
In atrial fibrillation that rhythmic contraction is lost and blood can collect in the left atrial appendage and form a clot.
For older patients, atrial fibrillation (AF) is a common rhythm disturbance where the top chambers of the heart (atria) do not beat regularly.
The symptoms of AF vary from mild fatigue to dizziness to chest pain or difficulty breathing. Some patients feel their heart palpitating, while others are unaware of the change in heart rate. However, whether AF causes symptoms or not the blood inside the pouch (appendage) is not ejected as it is during normal rhythm and blood clots may form in the pouch as a consequence.
These clots can pass into the left atrium and then travel to the brain causing a stroke. It is estimated that the clots which cause stroke in patients with AF originate in the left atrial appendage 90% of the time.
Most patients who develop AF are required to take "blood thinners" such as warfarin for the rest of their lives to prevent blood clots forming. Warfarin can be a difficult medication to take as there are many interactions with food items, alcohol and other drugs.
The medication dose may need frequent review and blood testing is required at least monthly. There are also significant bleeding risks while taking warfarin, particularly as patients get older. Newer "blood thinners" which are easier to take are becoming available. The bleeding risks with the newer agents are less than with warfarin but still not negligible.

An alternative approach to reduce the risk of blood clot formation in the left atrial appendage is to remove the appendage from circulation by closing it off using a form of “plug” such as the Watchman device.